Ketoacidosis, specifically diabetic ketoacidosis (DKA), is a severe and potentially life-threatening complication of diabetes, particularly prevalent in individuals with type 1 diabetes. This condition arises when the body begins to break down fat at an accelerated rate, leading to the production of ketones and a subsequent accumulation of acids in the blood. Understanding the causes and mechanisms behind ketoacidosis is crucial for effective management and prevention. This comprehensive article explores the underlying factors that contribute to ketoacidosis in type 1 diabetes, detailing the biochemical processes, risk factors, and strategies for prevention and treatment.
The Biochemical Basis of Ketoacidosis
To comprehend what causes ketoacidosis, it is essential to understand the biochemical processes involved in the condition.
The Role of Insulin
Insulin is a hormone produced by the pancreas that facilitates the uptake of glucose into cells for energy. In individuals with type 1 diabetes, the body’s immune system attacks and destroys the insulin-producing beta cells in the pancreas, leading to a deficiency of insulin.
Insulin Deficiency: Without adequate insulin, glucose cannot effectively enter cells. As a result, blood glucose levels rise (hyperglycemia), and cells are deprived of their primary energy source.
The Shift to Fat Metabolism
In the absence of sufficient insulin, the body starts to rely on fat stores for energy.
Lipolysis: The breakdown of fat (lipolysis) releases fatty acids into the bloodstream. These fatty acids are transported to the liver, where they are metabolized to produce ketones.
Ketogenesis: The liver converts fatty acids into ketone bodies (acetoacetate, beta-hydroxybutyrate, and acetone) as an alternative energy source. However, excessive ketone production leads to a buildup of acids in the blood, resulting in ketoacidosis.
The Development of Metabolic Acidosis
The accumulation of ketones leads to metabolic acidosis, a condition characterized by a decrease in blood pH.
Acidosis: Ketone bodies are acidic, and their accumulation lowers blood pH, leading to metabolic acidosis. This imbalance can affect various bodily systems and lead to symptoms such as nausea, vomiting, and abdominal pain.
Compensatory Mechanisms: The body attempts to compensate for metabolic acidosis through respiratory compensation (increased breathing rate to expel carbon dioxide) and renal compensation (increased excretion of acids in the urine). However, these mechanisms may not always be sufficient, especially if ketoacidosis is severe.
Common Causes and Triggers of Ketoacidosis in Type 1 Diabetes
Several factors can precipitate ketoacidosis in individuals with type 1 diabetes. Understanding these triggers is essential for prevention and management.
Inadequate Insulin Administration
Missed Insulin Doses: One of the most common causes of ketoacidosis is the omission of insulin doses. This can occur due to various reasons, including forgetfulness, lack of access to insulin, or mismanagement of insulin therapy.
Insulin Pump Malfunctions: For individuals using insulin pumps, malfunctions or interruptions in insulin delivery can lead to inadequate insulin levels and subsequent ketoacidosis.
Acute Illness or Infection
Infections: Acute illnesses or infections, such as influenza or urinary tract infections, can increase the body’s demand for insulin. The stress response to infection can exacerbate hyperglycemia and trigger ketoacidosis.
Fever and Dehydration: Infections can also lead to dehydration, which can further concentrate blood glucose and ketone levels, increasing the risk of ketoacidosis.
Stress and Emotional Factors
Physical Stress: Physical stress, such as trauma or surgery, can elevate stress hormones (e.g., cortisol) that counteract the effects of insulin. This can lead to increased blood glucose and ketone production.
Emotional Stress: Emotional stress, including anxiety or depression, can also impact blood glucose control. Stress-induced hormonal changes can contribute to the development of ketoacidosis.
Dietary Factors
Inadequate Carbohydrate Intake: Insufficient carbohydrate intake can lead to inadequate glucose availability, prompting the body to rely more heavily on fat metabolism and ketone production.
High-Fat Diet: A diet excessively high in fats may exacerbate ketone production, increasing the risk of ketoacidosis, especially if insulin levels are not appropriately managed.
Poor Diabetes Management
Uncontrolled Diabetes: Long-standing or poorly controlled diabetes can increase the risk of ketoacidosis. Chronic hyperglycemia and inadequate insulin management can contribute to the development of ketones.
Lack of Monitoring: Inadequate monitoring of blood glucose and ketone levels can delay the detection of ketoacidosis, leading to more severe complications.
Signs and Symptoms of Ketoacidosis
Recognizing the signs and symptoms of ketoacidosis is critical for early intervention and treatment.
Classic Symptoms
Polyuria and Polydipsia: Increased urination (polyuria) and excessive thirst (polydipsia) are common symptoms due to elevated blood glucose levels and subsequent dehydration.
Nausea and Vomiting: Gastrointestinal symptoms such as nausea and vomiting can occur as a result of metabolic acidosis and irritation from ketones.
Abdominal Pain: Abdominal discomfort or pain may be experienced due to the body’s response to acidosis and gastrointestinal effects.
Fruity Breath Odor: A distinctive fruity or acetone-like odor on the breath is a characteristic sign of ketoacidosis, resulting from the accumulation of acetone.
Severe Symptoms
Confusion and Altered Mental Status: Severe ketoacidosis can lead to confusion, disorientation, or even coma due to the effects of metabolic acidosis on brain function.
Rapid Breathing: To compensate for metabolic acidosis, individuals may exhibit rapid, deep breathing (Kussmaul respirations) to expel carbon dioxide and reduce acidity.
Fatigue and Weakness: Generalized fatigue, weakness, and lethargy may be present due to the body’s metabolic disturbances and dehydration.
Diagnosis of Ketoacidosis
Accurate diagnosis of ketoacidosis involves assessing clinical symptoms, blood glucose levels, and ketone concentrations.
Blood Glucose Testing
Hyperglycemia: Elevated blood glucose levels are a hallmark of ketoacidosis. Blood glucose measurements are used to confirm the presence of hyperglycemia.
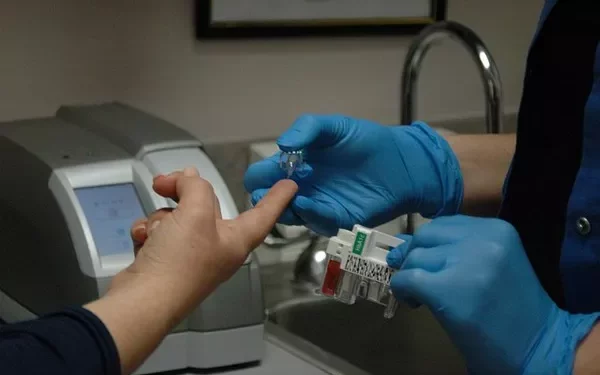
Ketone Testing
Urine Ketones: Urine ketone tests can provide an indication of ketone levels in the body. Positive results suggest increased ketone production.
Blood Ketones: Blood ketone testing is more precise and can measure the concentration of ketone bodies (e.g., beta-hydroxybutyrate) directly in the bloodstream.
Arterial Blood Gas (ABG) Analysis
Metabolic Acidosis: An ABG analysis can assess blood pH and bicarbonate levels, confirming the presence of metabolic acidosis associated with ketoacidosis.
Treatment and Management of Ketoacidosis
Effective management of ketoacidosis involves addressing the underlying causes, correcting metabolic imbalances, and providing supportive care.
Insulin Therapy
Intravenous Insulin: Immediate treatment typically involves intravenous insulin administration to reduce blood glucose levels and halt ketone production.
Insulin Dose Adjustment: Ongoing insulin therapy is adjusted based on blood glucose and ketone levels to achieve optimal control and prevent recurrence.
Fluid and Electrolyte Replacement
Rehydration: Intravenous fluids are administered to address dehydration, restore electrolyte balance, and improve circulation.
Electrolyte Management: Electrolyte imbalances, such as low potassium levels, are corrected to support normal cellular function and prevent complications.
Monitoring and Support
Continuous Monitoring: Continuous monitoring of blood glucose, ketone levels, and vital signs is essential for assessing treatment effectiveness and adjusting therapy as needed.
Supportive Care: Supportive care includes addressing symptoms such as nausea and abdominal pain, and providing education on preventing future episodes of ketoacidosis.
Preventing Ketoacidosis in Type 1 Diabetes
Preventing ketoacidosis involves proactive management and regular monitoring to reduce the risk of severe complications.
Consistent Insulin Management
Adherence to Therapy: Consistent administration of insulin as prescribed is critical for maintaining blood glucose control and preventing ketoacidosis.
Monitoring Insulin Delivery: Regular checks of insulin pumps or other delivery devices ensure proper function and prevent interruptions in insulin therapy.
Regular Monitoring and Testing
Blood Glucose and Ketone Monitoring: Regular monitoring of blood glucose and ketone levels helps detect early signs of metabolic disturbances and allows for prompt intervention.
Sick Day Management: During illness or infection, close monitoring and adjustments to insulin therapy are necessary to manage increased glucose levels and prevent ketoacidosis.
Education and Awareness
Patient Education: Educating individuals with type 1 diabetes about the signs of ketoacidosis, its prevention, and the importance of adherence to therapy is crucial for effective management.
Support Networks: Engaging with support networks, including diabetes educators and healthcare providers, provides valuable resources and guidance for managing diabetes and preventing complications.
See also: What Blood Test For Hypoglycemia
Conclusion
Ketoacidosis is a serious complication of type 1 diabetes, arising from a complex interplay of biochemical, physiological, and behavioral factors. Understanding the causes of ketoacidosis, including insulin deficiency, stress, infection, and poor diabetes management, is essential for effective prevention and treatment. By addressing the underlying mechanisms and implementing comprehensive management strategies, individuals with type 1 diabetes can reduce the risk of ketoacidosis and improve their overall health and well-being. Ongoing education, monitoring, and support play a critical role in managing this condition and enhancing the quality of life for those affected.
Related topics:
What Is a Normal Blood Sugar Level for Type 1 Diabetes?