Sepsis is a severe and often life-threatening condition resulting from an infection that triggers a widespread inflammatory response throughout the body. This systemic reaction can lead to various complications, one of which is hyperglycemia, or elevated blood glucose levels. Understanding the relationship between sepsis and hyperglycemia is crucial for effective management and treatment of both conditions. In this article, we will explore how sepsis can cause hyperglycemia, the mechanisms behind this process, and the implications for patient care.
Understanding Sepsis
Sepsis occurs when the body’s response to an infection becomes dysregulated, leading to widespread inflammation, blood clotting, and impaired organ function. The condition can progress rapidly and may result in septic shock, characterized by a significant drop in blood pressure and potential multi-organ failure.
Sepsis is commonly caused by bacterial infections but can also result from infections with viruses, fungi, or parasites. The condition is diagnosed based on clinical criteria and laboratory tests, including blood cultures and markers of inflammation.
Hyperglycemia: An Overview
Hyperglycemia refers to elevated blood glucose levels, which can result from various factors, including diabetes mellitus, hormonal imbalances, and acute medical conditions. Persistent hyperglycemia can lead to complications such as cardiovascular disease, neuropathy, and nephropathy.
In the context of sepsis, hyperglycemia is not merely a symptom but a significant aspect of the condition that can influence patient outcomes. Understanding how sepsis contributes to hyperglycemia involves examining the interplay between inflammatory responses, hormonal changes, and metabolic disturbances.
Mechanisms Linking Sepsis to Hyperglycemia
Sepsis-induced hyperglycemia is a complex process involving several interconnected mechanisms. Here are the key pathways through which sepsis can lead to elevated blood glucose levels:
1. Stress-Induced Hormonal Changes
During sepsis, the body experiences a significant stress response, which leads to the release of stress hormones such as cortisol, epinephrine, and norepinephrine. These hormones play a crucial role in the body’s response to infection but also have a profound impact on glucose metabolism.
Cortisol: Cortisol, a glucocorticoid hormone produced by the adrenal glands, increases blood glucose levels by promoting gluconeogenesis (the production of glucose from non-carbohydrate sources) in the liver. It also reduces glucose uptake by peripheral tissues, contributing to hyperglycemia.
Epinephrine and Norepinephrine: These catecholamines increase glucose production and release from the liver while inhibiting insulin secretion and action. This results in elevated blood glucose levels, especially in the context of systemic infection and inflammation.
2. Insulin Resistance
Sepsis is associated with a state of insulin resistance, where the body’s cells become less responsive to the effects of insulin. This resistance is mediated by several factors:
Inflammatory Cytokines: During sepsis, inflammatory cytokines such as tumor necrosis factor-alpha (TNF-alpha) and interleukin-6 (IL-6) are released into the bloodstream. These cytokines interfere with insulin signaling pathways, reducing the effectiveness of insulin in promoting glucose uptake by cells.
Cellular Stress: The systemic inflammation and oxidative stress associated with sepsis can impair the function of insulin receptors on cell membranes. This further contributes to reduced glucose uptake and increased blood glucose levels.
3. Hyperglycemia as a Compensatory Response
Hyperglycemia during sepsis can also be viewed as a compensatory response to the infection. Elevated blood glucose levels provide an alternative energy source for the body’s cells during a stressful and energy-demanding situation. However, this response can be detrimental if it becomes excessive or persistent.
Energy Supply: During sepsis, the body’s demand for energy increases due to the heightened metabolic rate and the need to support immune function. Elevated glucose levels can help meet these increased energy demands, although this comes at the cost of exacerbating hyperglycemia.
4. Altered Gluconeogenesis and Glycogenolysis
Sepsis affects liver function and glucose metabolism, leading to alterations in gluconeogenesis (the production of glucose from non-carbohydrate sources) and glycogenolysis (the breakdown of glycogen into glucose).
Increased Gluconeogenesis: The liver produces more glucose through gluconeogenesis in response to the stress of sepsis. This process is driven by elevated cortisol levels and the need to provide additional energy to the body’s cells.
Glycogenolysis: The breakdown of glycogen stores in the liver is also increased during sepsis, contributing to higher blood glucose levels. This process is influenced by stress hormones and the need to mobilize glucose rapidly.
Clinical Implications of Sepsis-Induced Hyperglycemia
The presence of hyperglycemia in septic patients has significant clinical implications. Managing hyperglycemia in the context of sepsis is crucial for improving patient outcomes and reducing complications. Here are some key considerations:
1. Impact on Patient Outcomes
Increased Mortality Risk: Hyperglycemia in septic patients is associated with higher mortality rates. Elevated blood glucose levels can exacerbate the inflammatory response, impair immune function, and increase the risk of multi-organ failure.
Organ Dysfunction: Persistent hyperglycemia can contribute to organ dysfunction by impairing blood flow, increasing oxidative stress, and disrupting normal metabolic processes. This can lead to complications such as acute kidney injury and cardiovascular instability.
2. Management Strategies
Effective management of hyperglycemia in septic patients involves a combination of strategies aimed at controlling blood glucose levels and addressing the underlying infection. Key approaches include:
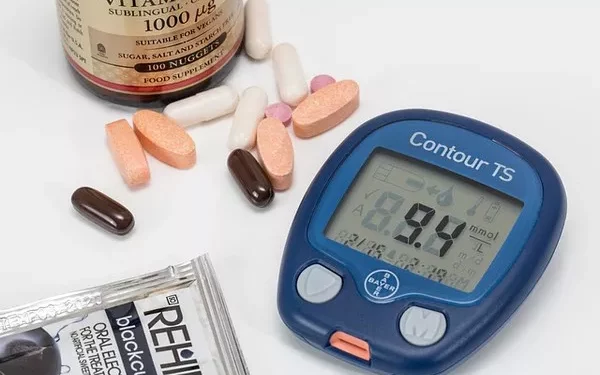
Glycemic Control: Tight glycemic control is essential for improving outcomes in septic patients. This can be achieved through regular monitoring of blood glucose levels and the use of insulin therapy to maintain glucose levels within a target range.
Insulin Therapy: Insulin is the primary treatment for managing hyperglycemia in sepsis. Continuous intravenous insulin infusion is often used in critically ill patients to achieve precise glucose control. Insulin therapy should be carefully managed to avoid both hyperglycemia and hypoglycemia.
Addressing Underlying Infection: Effective management of the underlying infection is crucial for controlling sepsis and reducing hyperglycemia. This involves the use of appropriate antibiotics or antifungal agents, supportive care, and interventions to address the source of infection.
Monitoring and Supportive Care: Regular monitoring of blood glucose levels, organ function, and other clinical parameters is essential for managing hyperglycemia and sepsis. Supportive care measures, including fluid resuscitation and hemodynamic support, may also be required.
3. Preventing Hyperglycemia-Related Complications
Preventing complications related to hyperglycemia in septic patients involves a proactive approach to glucose management and early intervention. Strategies include:
Early Recognition: Identifying and addressing hyperglycemia early in the course of sepsis can help prevent complications and improve patient outcomes. Regular glucose monitoring and prompt treatment adjustments are crucial.
Personalized Treatment: Tailoring treatment plans to the individual needs of each patient is essential for effective management. This includes adjusting insulin doses, monitoring for potential side effects, and addressing any underlying health conditions.
Research and Future Directions
Ongoing research aims to improve our understanding of the relationship between sepsis and hyperglycemia and to develop more effective management strategies. Key areas of focus include:
Mechanistic Studies: Research into the molecular and cellular mechanisms underlying sepsis-induced hyperglycemia can provide insights into potential therapeutic targets and interventions.
Glycemic Control Guidelines: Developing evidence-based guidelines for glycemic control in septic patients can help standardize care and improve outcomes. This includes determining optimal glucose targets and treatment protocols.
Novel Therapeutic Approaches: Investigating new therapeutic approaches, such as medications that target specific pathways involved in insulin resistance and hyperglycemia, may offer additional options for managing sepsis-induced hyperglycemia.
See also: How to Manage Hyperglycemia Effectively
Conclusion
Sepsis-induced hyperglycemia is a complex and multifaceted condition resulting from the interplay between stress hormones, insulin resistance, and metabolic disturbances. Understanding how sepsis contributes to elevated blood glucose levels is essential for effective management and improving patient outcomes.
Hyperglycemia in septic patients poses significant clinical challenges and can impact patient outcomes by increasing mortality risk and contributing to organ dysfunction. Effective management involves a combination of glycemic control, insulin therapy, addressing the underlying infection, and supportive care.
Ongoing research and advancements in treatment strategies will continue to enhance our understanding of sepsis and hyperglycemia, ultimately leading to better management and improved outcomes for patients with this serious condition. By addressing hyperglycemia proactively and providing comprehensive care, healthcare professionals can optimize patient outcomes and reduce the impact of sepsis-induced hyperglycemia.
Related topics: