Hemoglobin A1c (HbA1c) is a crucial marker for monitoring blood glucose control in individuals with diabetes. It reflects the average blood glucose levels over the past two to three months, and maintaining it within a target range is vital for reducing the risk of long-term diabetes-related complications. In this article, we explore evidence-based strategies for controlling HbA1c, emphasizing lifestyle modifications, medical management, and the importance of regular monitoring to achieve optimal diabetes management.
Understanding HbA1c and Its Significance
HbA1c is formed when glucose binds to hemoglobin, a protein in red blood cells. The more glucose in the blood, the higher the HbA1c level. HbA1c is expressed as a percentage, with a normal range being between 4% and 5.6%. For individuals with diabetes, the goal is usually to keep HbA1c levels below 7%, although this target may vary based on individual factors such as age, comorbidities, and risk of hypoglycemia.
When HbA1c levels are consistently high, it indicates poor blood glucose control and an increased risk of complications such as heart disease, kidney damage, neuropathy, and retinopathy. Therefore, managing HbA1c is essential not only for preventing complications but also for improving overall quality of life.
1. Lifestyle Modifications: The Foundation of HbA1c Control
Lifestyle changes play a central role in managing blood glucose levels and achieving a healthy HbA1c. Diet, physical activity, and weight management are three critical components that directly influence blood sugar regulation.
Healthy Eating: A Balanced Approach to Carbohydrate Intake
Dietary modifications are among the most effective ways to control HbA1c. Individuals with diabetes must prioritize a balanced diet that helps maintain stable blood glucose levels.
Carbohydrate Counting: Carbohydrates have the most significant impact on blood sugar levels. By counting carbohydrates and understanding their glycemic index (GI), individuals can better predict and control postprandial blood glucose spikes. Low-GI foods such as whole grains, legumes, and non-starchy vegetables are beneficial for steady glucose release.
Portion Control: Managing portion sizes is essential for avoiding excessive calorie and carbohydrate intake. Eating smaller, more frequent meals can help prevent large blood sugar fluctuations.
Focus on Fiber: Dietary fiber slows the absorption of sugar and improves insulin sensitivity. A diet high in fiber, particularly soluble fiber found in fruits, vegetables, and whole grains, can help reduce HbA1c levels.
Limit Processed Foods and Sugars: Processed foods, sugary snacks, and sugary beverages can cause rapid spikes in blood glucose. Reducing or eliminating these items from the diet is crucial for blood glucose management.
Regular Physical Activity: Exercise as a Blood Glucose Regulator
Exercise is an excellent way to lower blood sugar levels and improve insulin sensitivity. Regular physical activity helps muscles use glucose for energy, which can lower circulating blood glucose levels.
Aerobic Exercise: Activities like walking, cycling, swimming, and running help improve cardiovascular health and assist in glucose metabolism. At least 150 minutes of moderate-intensity aerobic activity per week is recommended.
Strength Training: Building muscle mass through resistance exercises helps increase insulin sensitivity and glucose uptake by cells. Strength training exercises should be incorporated at least two days per week.
Consistency Is Key: The more regularly an individual engages in physical activity, the more significant the impact on blood glucose control. Consistency in both exercise type and duration is essential for long-term success.
Achieving and Maintaining a Healthy Weight
Overweight and obesity are major risk factors for insulin resistance, making it harder for the body to maintain stable blood glucose levels. Losing even a small amount of weight can significantly improve HbA1c control.
Calorie Reduction: Reducing caloric intake through portion control and mindful eating can help promote weight loss. A calorie deficit, where fewer calories are consumed than expended, is essential for weight management.
Behavioral Modifications: Adopting healthier eating habits and increasing physical activity are key to achieving sustainable weight loss. Regular monitoring of food intake and exercise can help individuals stay on track.
Long-Term Commitment: Sustainable weight loss is more important than rapid weight loss. Small, gradual changes in lifestyle habits yield better long-term results for blood sugar management and overall health.
2. Medical Management: Pharmacological Interventions for HbA1c Control
While lifestyle changes form the cornerstone of diabetes management, pharmacological treatment may be necessary for those who struggle to achieve target HbA1c levels with diet and exercise alone. Various classes of diabetes medications can help lower blood glucose levels, and the choice of medication depends on individual patient factors, such as comorbidities, age, and treatment goals.
Insulin Therapy
Insulin is the primary treatment for individuals with type 1 diabetes and may also be used for individuals with type 2 diabetes who are unable to control blood glucose with oral medications.
Basal Insulin: Long-acting insulin is used to maintain a steady baseline level of insulin in the body throughout the day and night.
Bolus Insulin: Rapid-acting insulin is taken at meal times to help control the immediate rise in blood glucose after eating.
Insulin Pumps: Insulin pumps provide a continuous infusion of insulin and may offer greater flexibility and better blood glucose control.
Oral Medications for Type 2 Diabetes
There are several classes of oral medications available to help manage blood glucose in type 2 diabetes. Some of the most commonly prescribed include:
Metformin: The first-line treatment for type 2 diabetes, metformin works by improving insulin sensitivity and reducing glucose production by the liver. It is often effective in lowering HbA1c when combined with lifestyle changes.
Sulfonylureas: These medications stimulate the pancreas to release more insulin. While effective in lowering blood glucose, they can increase the risk of hypoglycemia.
DPP-4 Inhibitors: These drugs work by increasing the levels of incretin hormones, which help regulate insulin production and glucose metabolism.
SGLT2 Inhibitors: SGLT2 inhibitors prevent the kidneys from reabsorbing glucose, promoting its excretion in urine. These medications have the added benefit of reducing cardiovascular risk and promoting weight loss.
GLP-1 Receptor Agonists
GLP-1 receptor agonists stimulate insulin secretion, inhibit glucagon release, and slow gastric emptying, leading to improved blood glucose control and reduced appetite. These medications are administered via injection and have been shown to improve HbA1c levels and promote weight loss.
Insulin Sensitizers
Medications like thiazolidinediones (TZDs) improve the body’s sensitivity to insulin, helping cells use glucose more effectively. While effective, they may have side effects such as weight gain and fluid retention.
Combination Therapies
For individuals whose HbA1c remains elevated despite monotherapy, combination therapy may be necessary. This can involve combining oral medications or adding insulin or injectable medications to a treatment regimen to achieve better blood glucose control.
3. The Role of Continuous Glucose Monitoring (CGM)
Continuous glucose monitoring (CGM) systems provide real-time blood glucose readings throughout the day and night, offering a comprehensive picture of glucose fluctuations. CGM devices can be particularly helpful for individuals who struggle to maintain consistent HbA1c levels and wish to monitor their blood glucose more closely.
Data-Driven Decisions: CGM allows individuals to track how their glucose levels respond to meals, exercise, stress, and medications, enabling more informed decisions regarding insulin dosages and lifestyle adjustments.
Alerts for Hypoglycemia: CGM systems can send alerts when blood glucose levels are too low or too high, helping individuals take immediate action to prevent dangerous fluctuations.
Improved HbA1c Control: Studies have shown that CGM can lead to better HbA1c control by reducing both hyperglycemia and hypoglycemia, making it a valuable tool for people with diabetes.
4. Regular Monitoring and Professional Support
Frequent blood glucose monitoring is essential for effective diabetes management. Individuals with diabetes should work closely with healthcare professionals to set realistic goals for HbA1c control and adjust treatment plans as necessary.
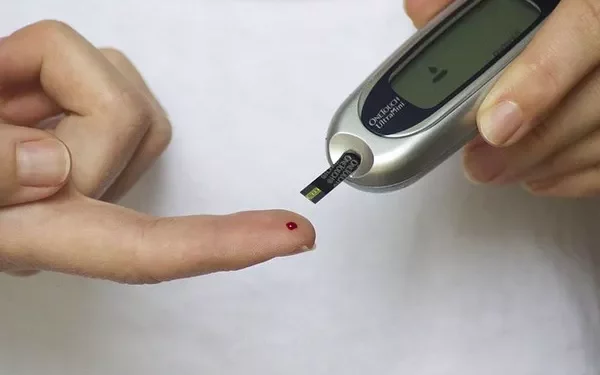
Self-Monitoring of Blood Glucose (SMBG)
Self-monitoring of blood glucose involves using a glucometer to check blood sugar levels at specific times of the day. This helps individuals understand how their diet, exercise, and medications impact their blood glucose levels.
Frequency of Testing: The frequency of testing should be tailored to the individual’s treatment plan. Those on insulin therapy may need to monitor blood glucose more frequently, while others with more stable blood glucose levels may test less often.
Record Keeping: Keeping a detailed log of blood glucose readings, meals, exercise, and medications can help identify patterns and guide adjustments in treatment.
Regular HbA1c Testing
In addition to daily blood glucose monitoring, HbA1c should be tested every three to six months to assess long-term glucose control. This allows individuals and their healthcare team to adjust treatment strategies as needed.
5. Psychological Support and Stress Management
Managing diabetes can be emotionally challenging, and stress can significantly impact blood glucose levels. Psychological support and stress management techniques are essential for improving both physical and mental well-being.
Behavioral Health Support: Counseling, support groups, or cognitive-behavioral therapy can help individuals cope with the psychological aspects of diabetes.
Mindfulness and Relaxation: Techniques such as meditation, deep breathing, and yoga can help reduce stress and improve insulin sensitivity.
Conclusion
Controlling HbA1c in diabetes is a multifaceted endeavor that requires a combination of lifestyle changes, medical management, and regular monitoring. By adopting a balanced diet, engaging in regular physical activity, and adhering to prescribed medications, individuals with diabetes can successfully manage their blood glucose levels and reduce the risk of complications. Continuous support from healthcare professionals and the use of advanced monitoring tools, such as CGM, further enhance the ability to maintain stable blood glucose levels and achieve long-term success in diabetes management.
Through a comprehensive, personalized approach to diabetes care, individuals can live healthier, more fulfilling lives while keeping their HbA1c within target ranges.
Related topics:
What are Pre-Diabetic Blood Glucose Levels