Glucose monitoring is a critical aspect of diabetes management. It helps individuals with diabetes keep their blood sugar levels within a target range, thereby preventing complications and maintaining overall health. Traditional glucose monitoring involves measuring blood glucose levels using a fingerstick and a glucose meter. However, advancements in technology have introduced continuous glucose monitoring (CGM) systems that measure interstitial glucose levels. Understanding the differences between interstitial glucose and blood glucose is essential for effective diabetes management.
Definition and Measurement
Blood Glucose: Blood glucose, or blood sugar, refers to the concentration of glucose present in the blood. It is the primary source of energy for the body’s cells and is tightly regulated by hormones such as insulin and glucagon. Blood glucose levels are typically measured using a glucose meter, which requires a small drop of blood obtained through a fingerstick.
Interstitial Glucose: Interstitial glucose refers to the glucose present in the interstitial fluid, the fluid that surrounds the cells in the tissues. Continuous glucose monitoring (CGM) systems measure interstitial glucose levels using a sensor inserted under the skin. The sensor continuously records glucose levels in the interstitial fluid and provides real-time data.
Physiological Differences
Blood Glucose: Blood glucose levels fluctuate throughout the day in response to various factors, including food intake, physical activity, medication, and stress. The measurement of blood glucose provides an immediate snapshot of the glucose levels in the bloodstream at the time of testing. It is a direct measurement and is considered the gold standard for diagnosing and managing diabetes.
Interstitial Glucose: Interstitial glucose levels also fluctuate in response to the same factors that affect blood glucose. However, there is a physiological lag between changes in blood glucose levels and corresponding changes in interstitial glucose levels. This lag, known as the “lag time,” typically ranges from 5 to 15 minutes. Despite this delay, interstitial glucose monitoring provides valuable trend data and can help predict changes in blood glucose levels.
Monitoring Methods
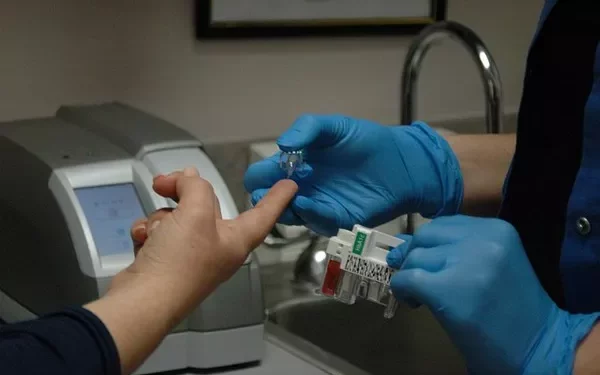
Blood Glucose Monitoring: Blood glucose monitoring is performed using a glucose meter. The process involves the following steps:
Wash and dry your hands to ensure cleanliness.
Use a lancet to prick the side of your fingertip and obtain a small drop of blood.
Apply the blood drop to a test strip inserted into the glucose meter.
The meter displays the blood glucose level within seconds.
Continuous Glucose Monitoring (CGM): CGM systems measure interstitial glucose levels using a sensor inserted under the skin, typically on the abdomen or the upper arm. The monitoring process involves the following steps:
Insert the sensor under the skin using an applicator.
Connect the sensor to a transmitter that sends data to a receiver or a compatible device, such as a smartphone.
The sensor continuously measures interstitial glucose levels and transmits the data at regular intervals, usually every 5 minutes.
The receiver or compatible device displays real-time glucose levels, trends, and alerts for high or low glucose levels.
Advantages and Limitations
Blood Glucose Monitoring:
Advantages:
- Provides direct and immediate measurement of blood glucose levels.
- Highly accurate and reliable for diagnosing and managing diabetes.
- Useful for making immediate treatment decisions, such as insulin dosing.
Limitations:
- Requires frequent fingersticks, which can be painful and inconvenient.
- Provides only single-point measurements, lacking trend information.
- Does not offer continuous monitoring or predictive insights.
Continuous Glucose Monitoring (CGM):
Advantages:
- Provides continuous, real-time monitoring of glucose levels.
- Offers valuable trend data and predictive insights.
- Reduces the need for frequent fingersticks.
- Alerts users to high or low glucose levels, enabling timely intervention.
- Can improve overall glucose control and reduce the risk of complications.
Limitations:
- Measures interstitial glucose, which may have a lag time compared to blood glucose.
- Requires sensor insertion and periodic calibration (depending on the CGM model).
- May have higher upfront costs compared to traditional glucose meters.
- Potential for sensor-related skin irritation or discomfort.
Clinical Implications
The differences between interstitial glucose and blood glucose have important clinical implications for diabetes management. Understanding these differences can help individuals with diabetes and healthcare providers make informed decisions about monitoring methods and treatment strategies.
Lag Time Considerations: The lag time between blood glucose and interstitial glucose levels means that CGM readings may not always reflect immediate changes in blood glucose. This is particularly relevant during periods of rapid glucose changes, such as after meals, during exercise, or when treating hypoglycemia. Healthcare providers and individuals using CGM systems should be aware of this lag and consider it when interpreting CGM data and making treatment decisions.
Trend Data and Predictive Insights: One of the significant advantages of CGM systems is the ability to provide trend data and predictive insights. By analyzing the patterns and trends in interstitial glucose levels, individuals with diabetes can identify factors that affect their glucose control and make proactive adjustments to their diet, physical activity, and medication. CGM systems can also alert users to impending high or low glucose levels, allowing for timely interventions to prevent severe hypoglycemia or hyperglycemia.
Improving Glycemic Control: Research has shown that the use of CGM systems can improve glycemic control and reduce the risk of diabetes-related complications. Continuous monitoring and trend data enable individuals to maintain glucose levels within their target range more effectively. For example, CGM can help identify nighttime hypoglycemia or hyperglycemia, which may go unnoticed with traditional blood glucose monitoring. By addressing these patterns, individuals can achieve more stable glucose levels and reduce the risk of long-term complications such as cardiovascular disease, neuropathy, and retinopathy.
Patient Considerations
Individual Preferences: The choice between blood glucose monitoring and continuous glucose monitoring should consider individual preferences, lifestyle, and diabetes management goals. Some individuals may prefer the convenience and reduced fingersticks offered by CGM systems, while others may prioritize the immediate accuracy of blood glucose monitoring for certain situations, such as insulin dosing.
Cost and Insurance Coverage: The cost of CGM systems can be a consideration for many individuals. While the initial cost of a CGM system may be higher than a traditional glucose meter, the long-term benefits and potential cost savings from improved glycemic control and reduced complications should be weighed. Insurance coverage for CGM systems varies, and individuals should check with their insurance providers to understand their coverage options.
Education and Training: Proper education and training are essential for effectively using both blood glucose monitors and CGM systems. Healthcare providers should provide comprehensive training on how to use the devices, interpret the data, and make informed treatment decisions. Ongoing support and follow-up can help individuals with diabetes optimize their use of glucose monitoring technologies.
Future Directions in Glucose Monitoring
Advancements in glucose monitoring technologies continue to evolve, with ongoing research and development aimed at improving accuracy, convenience, and user experience. Some future directions in glucose monitoring include:
Non-Invasive Glucose Monitoring: Researchers are exploring non-invasive methods for glucose monitoring that do not require fingersticks or sensor insertion. These methods may include wearable devices that use light or other technologies to measure glucose levels through the skin.
Closed-Loop Systems: Closed-loop systems, also known as artificial pancreas systems, combine CGM with insulin pumps to automate insulin delivery based on real-time glucose readings. These systems aim to maintain glucose levels within a target range with minimal user intervention.
Improved Sensor Technology: Advances in sensor technology are focused on improving the accuracy, reliability, and lifespan of CGM sensors. This includes reducing the lag time between blood glucose and interstitial glucose measurements and enhancing sensor durability.
See also: What are Symptoms of Juvenile Diabetes
Conclusion
Understanding the difference between interstitial glucose and blood glucose is fundamental for effective diabetes management. While blood glucose monitoring provides immediate and direct measurements, continuous glucose monitoring offers valuable trend data and predictive insights. Both methods have their advantages and limitations, and the choice between them should be based on individual preferences, lifestyle, and diabetes management goals.
By leveraging the strengths of each monitoring method and staying informed about advancements in glucose monitoring technologies, individuals with diabetes can achieve better glycemic control, reduce the risk of complications, and improve their overall quality of life. Proper education, training, and support from healthcare providers play a crucial role in optimizing the use of glucose monitoring devices and ensuring successful diabetes management.
Related topics:
Flash VS Continuous Glucose Monitoring : What’s the Difference